Chiropractic Care for Acute Injuries
In the floor of the main hall of the Jordan Hall of Science at the University of Notre Dame there is a mosaic medallion, which states:
“Nothing in Biology Makes Sense Except in the Light of Evolution”
This saying is from Ukrainian-American Geneticist and Evolutionary Biologist, Theodosius Dobzhansky (1900-1975). Dobzhansky originally made this statement in a 1973 article.
Theodosius Dobzhansky was published widely in books and in peer reviewed scientific journals, including one of the most important books ever written, Genetics and the Origin of Species (1). Understanding the implications of this concept is key to understanding the reason humans have always needed and had available mechanically based healthcare, including chiropractic spinal manipulation.
•••••
Pain is a huge problem in America. Recent publications estimate that about half of the adults in America suffer from chronic pain (2). The primary body location for chronic pain is, by far, the low back (3).
Chiropractors treat spine pain. Recent statistics indicate that 63% of patients that initially seek chiropractic care do so for low back pain; another 30% do so for neck pain (4). Overwhelming evidence shows the substantial benefits of chiropractic spinal adjusting in the management of spinal pain problems (4, 5, 6, 7, 8, 9, 10, 11, 12, 13).
Almost any intervention will help acute pain: rest, ice, heat, drugs, herbs, homeopathy, manipulation, acupuncture, physical therapy, massage, etc. Yet, the majority of chiropractic patients suffer from chronic pain. The chiropractic degree is “DC,” which stands for Doctor of Chiropractic. Chiropractic instructors often note that DC could stand for “Doctor of Chronic Pain.”
Chiropractic care is mechanical care. Chiropractors evaluate the ways in which the body lives, exists, and functions in a gravity environment. Problems that are identified are managed by the application of specific line-of-drive forces that are called spinal adjusting. How does mechanical care impact the healing of an acute injury?
•••••
Sports in America (and worldwide) are popular for the athletes and fans, and also very big business. All levels of sports (professional, college, amateur, etc.) are coupled with hundreds of billions of dollars yearly. At the center of it all is the health and wellbeing of the athlete.
Injuries are a reality in all sports and at all levels of participation. The primary concern is the effective and successful management of acute injuries so that the athlete can return to competition. Follow this story from the Sports Pages of the newspaper USA Today “Medical Options Broaden the NFL” (14):
“Captain Munnerlyn is a believer.”
“The veteran Minnesota Viking cornerback thought he’d miss up to a month after injuring a hamstring in training camp. Then he visited ‘Dr. Josh,’ who worked on the injury once and left Munnerlyn thinking he’d just witnessed a miracle.”
“‘It was crazy. I’d never had it done before, but it got me back on the field in a week. Didn’t use anything. No machines, all hands. Wow, is this the Son of God’?”
“Josh Sandell is not a medical doctor. He’s a licensed chiropractor.”
The article continues to note how every NFL team now has a chiropractor, and that often the chiropractor is the busiest member of the athlete’s health care team.
Evolutionary Biology
The relevance of acute injury care to evolutionary biology is discussed in reference books on pathology, orthopedics, physiology, and immunology (15, 16, 17, 18, 19, 20, 21, 22, 23, 24). This is the basic premise:
- Throughout history, the primary killer of humans was microbes.
- Humans evolve mechanisms to increase rates of survival against microbes; consequently, these mechanisms also increased the human ability to reproduce, ensuring the survivability of our species.
- Adverse microbes damage tissues, resulting in an inflammatory cascade. The inflammatory cascade, in turn, would quickly activate a cellular process of fibrosis. The fibrosis would “wall off” the causative microbes from the adjacent tissues and systems, reducing the spread of the pathogens until the time-delayed adaptive immune response could initiate an elaborate specific response.
- Many things other than infection activate the acute inflammatory cascade: trauma, repetitive mechanical stress, chemicals, allergies, metabolic imbalances, autoimmunity, etc.
- The body does not distinguish the different initiators of inflammation from each other, and assumed they are secondary to infection.
- “Walling off” tissues in the absence of infection serves no selective advantages. Rather, it is deleterious because it creates local mechanical problems. These mechanical problems are biomechanically and neuro-biomechanically harmful to the subject.
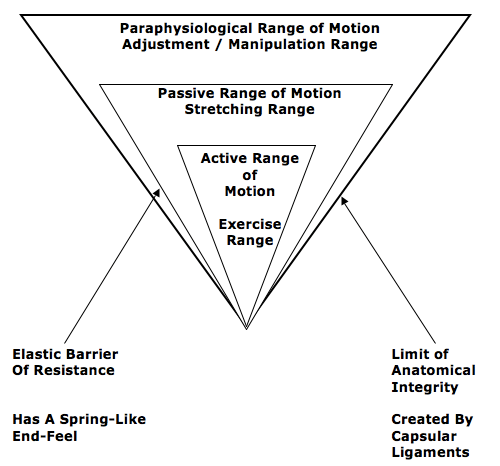
- These adverse biomechanical and neuro-biomechanical tissue changes are improved with various applications of mechanical care. A unique application of mechanical care is the specific line-of-drive adjustments delivered by chiropractors. The chiropractic adjustment has the unique ability to remodel fibrotic tissue changes that exist in the periarticular paraphysiological space, and it accomplishes this without adding to any adverse tissue stress.
Selected supportive quote include:
“The inflammatory reaction tends to prevent the dissemination of infection. Speaking generally, the more intense the reaction, the more likely the infection to be localized.” (15)
•••
“Inflammation is the most common, the most carefully studied, and the most important of the changes that the body undergoes as the result of disease.” (16)
•••
“Inflammation is the most common and fundamental pathological reaction.”
The agents leading to inflammation include “microbial, immunologic, physical, chemical, or traumatic.”
“The proliferative activity, leading to the production of abundant scar tissue, may in itself be distinctly harmful.” (17)
•••
“Inflammation serves to destroy, dilute, or wall-off the injurious agent.”
“Without inflammation, bacterial infections would go unchecked.”
“Reparative efforts may lead to disfiguring scars, fibrous bonds that limit the mobility of joints, or masses of scar tissue that hamper the function of organs.” (18)
•••
“The excessive reaction of tissues to an injury is conditioned by the overriding needs of a process designed to limit bacterial invasion. If there is to be only one pattern of response, it must be suited to the graver of the two possible traumas. However, elaborate preparation for preventing the spread of bacteria is not only pointless after an aseptic injury, but is so excessive as to prove harmful in itself. The principle on which the treatment of post-traumatic inflammation is based is that the reaction of the body to an injury unaccompanied by infection is always too great.” (19)
•••
“It is important to realize that the body’s initial reaction to an injury is similar to its reaction to an infection. The reaction is termed inflammation and may manifest macroscopically (such as after an acute injury) or at a microscopic level, with the latter occurring particularly in chronic overuse conditions.” (20)
•••
“One of the first results of inflammation is to ‘wall off’ the area of injury from the remaining tissues.”
“This walling-off process delays the spread of bacteria or toxic products.” (21)
•••
“There are two important consequences of being a warm-blooded animal. One is that body fluids make optimal culture media for bacteria. It is to the animal’s advantage, therefore, to heal wounds with alacrity in order to reduce chances of infection.”
“The prompt development of granulation tissue forecasts the repair of the interrupted dermal tissue to produce a scar.” In addition to providing tensile strength, scars are believed to be a barrier to infectious migration. (22)
•••
“When our ancestors became bipedal, descending from the trees and walking the savanna, inflammation was actually an advantage. Inflammation is part of the reaction by the immune system to foreign invaders, which allowed our ancestors to survive stepping on dung, puncturing their feet, eating raw meat filled with pathogens, and sustaining wounds during hunts as well as while fighting with each other.”
“In all of these situations, mounting a robust inflammatory response protects against life-threatening infection.” (23)
•••
Inflammation is defined as “a curative reaction of organisms, and morbid symptoms are no other than the signs of struggle between the mesodermic cells and the microbes.”
“Pathogens, unlike the healthy cells in our own bodies, don’t like to stay in a particular area. They are built to cross borders, push into virgin tissue, spread, eat, and replicate.”
“Once inside, the pathogen mingles with our cells, reproduces, makes a colony. At this point, one or more of a number of first-line immune system cells suspect danger. They are the constituents of a fire brigade. This is inflammation.”
“You need inflammation to protect against invaders.” BUT “In millions of people, excessive immune response is its own chronic disease.”
Pathogens “move around and through barriers in our bodies more easily that other cells.”
“The term for one of the key cell types stimulating regeneration of our tissues is fibroblast—highly versatile and hearty cells that proliferate and migrate to the site.”
“As the fibroblast cells come together, they form connective tissue, a bridge between the new and old tissue. At the wound site, the new tissue takes on a granular quality, hence its name granulation tissue. A kind of a tenacious web forms, a fibrous matrix that protects against invading pathogens.” (24)
The model presented supports that inflammation is a paradox. Inflammation can directly kill pathogens. Inflammation also triggers a fibrous response that walls-off infection so that the pathogens are less likely to spread and kill the host. Without inflammation, humans would die of infection. A strong inflammatory response is genetically selected, giving humans with such a response a survival advantage. Our ancestors genetically handed down these traits and modern humans possess them. In a world prior to the availability of antibiotics, inflammation, with reactive walling-off fibrosis to contain pathogens, is desirable because it increases host survivability.
Infection is not the only cause of inflammation. Inflammation is also triggered by trauma, excessive tissue stress, chemicals, immunologic responses, and more. Human bodies cannot distinguish the different causes of inflammation from each other, and therefore they all trigger a fibrous response. “The resolution of inflammation in the body is fibrosis.”
This fibrous response is necessary when there is an infection, as it is life saving. However in an aseptic sterile injury or tissue stress, the fibrous response is excessive and it creates adverse mechanical deficits. These adverse mechanical deficits create tissue stiffness and limit the mobility of joints. These mechanical deficits impair local biomechanical function, affecting performance, generating pain, and accelerating degenerative changes.
•••••
Stages of Healing Following Soft Tissue Injury
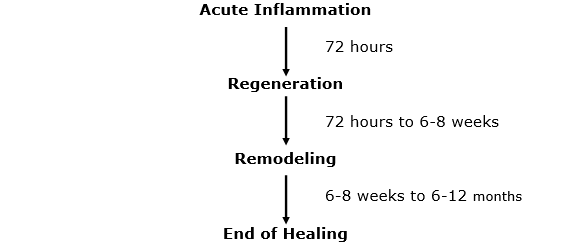
Soft tissues include ligaments, muscles, tendons, discs, and fascia. Essentially all tissues other than bone, but often injuries to the nerves and skin are excluded. For decades it has been understood that injured soft tissues heal over the period of about a year and in three distinct steps. A large range of reference textbooks and published studies are in agreement on these distinct steps (although some materials use slightly different terminology). (22, 25, 26, 27, 28, 29, 30, 31, 32, 33)
Phase 1: The Acute Inflammatory or Reaction Phase
This phase of healing begins immediately after injury and lasts up to about 72 hours. It is characterized by vasodilation, immune system activation of phagocytosis to remove debris, the release of inflammatory prostaglandins and cytokines.
Phase 2: The Repair or Regeneration Phase
This phase begins at about 48 hours and continues for about 6 weeks. This phase is characterized by the synthesis and deposition of collagen, which literally glues the margins of the healing breach together.
The collagen that is deposited in this phase is not fully oriented in the direction of tensile strength. Rather, is laid down in an irregular, non-physiological pattern.
Phase 3: The Remodeling Phase
This phase mingles with the terminal timing of the regeneration (phase 2). It may last up to 12 months or more.
It is during this phase that the collagen that is laid down during regeneration (phase 2) improves its alignment, strength, and functional capabilities.
The Concept of Motion
When a bone is broken (fracture), healing must take place in the presence of immobilization. In contrast, the healing of injured soft tissues requires controlled motion (19). Uncontrolled motion adds to injury. One cannot fix the injury of an automobile accident by getting involved in another collision. The application of controlled motion has many benefits in enhancing the quality and timing of soft tissue injury healing.
These statements emphasize the importance of the application of controlled motion for the healing of injured soft tissues:
“Her (Stearns) main conclusion on the mechanics of the formation of scar tissue was that external mechanical factors, were responsible for the development of the fibrillary network. At first the fibrils developed at random, but later they acquired a definite arrangement, apparently as a direct result of the mechanical factors. Of these factors, movement is obviously the most important and equally obvious it is most effective and least likely to cause pain before the fibrils have developed an abnormal firm attachment to neighboring structures. When free mobility was encouraged from the onset, the fibers in the scar were arranged lengthwise as in a normal ligament. Gentle passive movements do not detach fibrils from their proper formation at the healing breach but prevent their continued adherence at normal sites. The fact that the fibrils rapidly spread in all directions provides sufficient reason for beginning movements at the earliest possible moment; otherwise they develop into strong fibrous scars (adhesions) that so often cause prolonged disability after a sprain.” (34)
•••
“When pain is due to bacterial inflammation, Hilton’s advocacy of rest remains unchallenged and is today one of the main principles of medical treatment. When, however somatic pain is caused by inflammation due to trauma, his ideas require modification. When non-bacterial inflammation attacks the soft tissues that move, treatment by rest has been found to result in chronic disability, later, although the symptoms may temporarily diminish. Hence, during the present century, treatment by rest has given way to therapeutic movement in many soft tissue lesions.”
“Tension within the granulation tissue lines the cells up along the direction of stress. Hence, during the healing of mobile tissues, excessive immobilization is harmful. It prevents the formation of a scar strong in the important direction by avoiding the strains leading to due orientation of fibrous tissue and also allows the scar to become unduly adherent, e.g. to bone.” (19)
•••
“The injured tissues next undergo remodeling, which can take up to one year to complete in the case of major tissue disruption. The remodeling stage blends with the later part of the regeneration stage, which means that motion of the injured tissues will influence their structure when they are healed. This is one reason why it is necessary to consider using controlled motion during the recovery stage. If a limb is completely immobilized during the recovery process, the tissues may emerge fully healed but poorly adapted functionally, with little chance for change, particularly if the immobilization has been prolonged.”
“Early mobilization, guided by the pain response, promotes a more rapid return to full functional recovery.”
“It appears that the tensile strength of the collagen is quite specific to the forces imposed on it during the remodeling phase: i.e. the maximum strength will be in the direction of the forces imposed on the ligament.” (20)
•••
“Experimental and clinical studies demonstrate that early, controlled mobilization is superior to immobilization for primary treatment of acute musculoskeletal soft-tissue injuries and postoperative management.”
“The current literature on experimental acute soft-tissue injury speaks strongly for the use of early, controlled mobilization rather than immobilization for optimal heating.”
Experimentally induced ligament tears in animals heal much better with early, controlled mobilization than with immobilization.
“The superiority of early controlled mobilization has been especially clear in terms of quicker recovery and return to full activity without jeopardizing the subjective or objective long-term outcome.”
“The superiority of early controlled mobilization is especially apparent in terms of producing quicker recovery and return to full activity, without jeopardizing the long-term rehabilitative outcome.” (35)
•••
“Following this acute inflammatory phase and largely guided by the pain response of the patient, early mobilization is commenced, based upon the premise that the stress of movement on repairing collagen is largely responsible for the orientation and tensile strength of the tendons and ligaments.”
“The goal of stressing repairing tissues with controlled motion is to induce an adaptive response of functionally stronger connective tissues.”
“Collagen fiber growth and realignment can be stimulated by early tensile loading of muscle, tendon, and ligament.” (26)
•••
Following tendon injury, “micro-angiography, scanning electron microscopy, and light microscopy all demonstrated that the early mobilized group had normal appearance with a smooth surface and were free of adhesions.”
“These results demonstrated that forces and motion at the repair site provided by controlled early passive mobilization can accelerate healing of the repaired tendons, with reduced adhesions.”
“Controlled passive mobilization has been demonstrated to augment the quality of repair and stimulate a healing mode based on the tendon’s intrinsic healing capability.” (28)
•••
“The large scar tissue mass gradually remodels, likely under the influence of the mechanical environment.”
“Maturation of the scar tissue requires mechanical loading to continue the remodeling phase of healing.”
“Depriving healing ligaments of mechanical loading likely has a detrimental impact on healing outcome.” (30)
•••
“Mobilization for the treatment of soft tissue damage has also been found to decrease muscle atrophy, osteoporosis, adhesions, and joint stiffness following injury.”
To improve the quality of ligament healing after injury or surgery, controlled motion “can stimulate repair and restoration of function, and that treatment of ligament injuries with prolonged rest may actually delay recovery and adversely affect the tissue’s ability to repair itself.” (33)
Summary
In “light of evolutionary biology,” when inflammation is caused by non-infectious mechanisms, the fibrotic tissue response is excessive, resulting in mechanical harm to the host. This tissue fibrosis is minimized with early persistent controlled mobilization.
Spinal manipulation is a form of passive controlled motion that mechanically influences more tissue than does either active or passive motions (5). When specifically and carefully applied by a trained provider, such as a chiropractor, spinal manipulation is superior to other therapies at introducing controlled motion into injured soft tissues. The details presented here show value for the introduction of controlled motion in all three phases of soft tissue healing.
REFERENCES
- Dobzhansky T; Genetics and the Origin of Species; Columbia University Press; 1937, 1941, 1951.
- Foreman J; A Nation in Pain; Healing Our Biggest Health Problem; Oxford University Press; 2014.
- Wang S; Why Does Chronic Pain Hurt Some People More?; Wall Street Journal; October 7, 2013.
- Adams J, Peng W, Cramer H, Sundberg T, Moore C; The Prevalence, Patterns, and Predictors of Chiropractic Use Among US Adults; Results From the 2012 National Health Interview Survey; Spine; December 1, 2017; Vol. 42; No. 23; pp. 1810–1816.
- Kirkaldy-Willis WH, Cassidy JD; Spinal Manipulation in the Treatment of Low Back Pain; Canadian Family Physician, March 1985; Vol. 31; pp. 535-540.
- Meade TW, Dyer S, Browne W, Townsend J, Frank OA; Low back pain of mechanical origin: Randomized comparison of chiropractic and hospital outpatient treatment; British Medical Journal; June 2, 1990; Vol. 300; pp. 1431-1437.
- Woodward MN, Cook JCH, Gargan MF, Bannister GC; Chiropractic treatment of chronic ‘whiplash’ injuries; Injury; Vol. 27; No. 9; November 1996; pp. 643-645.
- Khan S, Cook J, Gargan M, Bannister G; A symptomatic classification of whiplash injury and the implications for treatment; The Journal of Orthopaedic Medicine; Vol. 21; No. 1; 1999, pp. 22-25.
- Giles LGF, Muller R; Chronic Spinal Pain: A Randomized Clinical Trial Comparing Medication, Acupuncture, and Spinal Manipulation; Spine; July 15, 2003; Vol. 28; No.14; pp. 1490-1502.
- Muller R, Giles LGF; Long-Term Follow-up of a Randomized Clinical Trial Assessing the Efficacy of Medication, Acupuncture, and Spinal Manipulation for Chronic Mechanical Spinal Pain Syndromes; Journal of Manipulative and Physiological Therapeutics, January 2005; Vol. 28; No. 1; pp. 3-11.
- Kirkaldy-Willis WH; Managing Low Back Pain; Churchill Livingstone; 1983.
- Cifuentes M, Willetts J, Wasiak R; Health Maintenance Care in Work-Related Low Back Pain and Its Association With Disability Recurrence; Journal of Occupational and Environmental Medicine; April 14, 2011; Vol. 53; No. 4; pp. 396-404.
- Senna MK, Machaly SA; Does Maintained Spinal Manipulation Therapy for Chronic Nonspecific Low Back Pain Result in Better Long-Term Outcome? Randomized Trial; SPINE; August 15, 2011; Vol. 36; No. 18; pp. 1427–1437.
- Pelissero T; Medical Options Broaden in NFL; USA Today; December 10, 2014; pp. 1C, 5C.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Lea and Febiger; 1952.
- Boyd W; PATHOLOGY: Structure and Function in Disease; Eighth Edition; Lea & Febiger; Philadelphia; 1970.
- Anderson WAD, Scotti TM; Synopsis of Pathology; Ninth Edition; The CV Mosby Company; 1976.
- Robbins SL, Cotran RS; PATHOLOGIC BASIS OF DISEASE; Second Edition; WB Saunders Company; Philadelphia; 1979.
- Cyriax J; Textbook of Orthopaedic Medicine, Diagnosis of Soft Tissue Lesions; Bailliere Tindall; Vol. 1; eighth edition; 1982.
- Roy S, Irvin R; Sports Medicine: Prevention, Evaluation, Management, and Rehabilitation; Prentice-Hall; 1983.
- Guyton A; Textbook of Medical Physiology; Saunders; 1986.
- Cohen IK, Diegelmann RF, Lindbald WJ; Wound Healing, Biochemical & Clinical Aspects; WB Saunders; 1992.
- Bredesen D; The End of Alzheimer’s: The First Program to Prevent and Reverse Cognitive Decline; Avery; 2017.
- Richtel M; An Elegant Defense: The Extraordinary New Science of the Immune System; William Morrow; 2019.
- Oakes BW; Acute Soft Tissue Injuries: Nature and Management; Australian Family Physician; July 1982; Vol. 10; No. 7 (supplement); pp. 3-16.
- Kellett J; Acute soft tissue injuries-a review of the literature; Medicine and Science of Sports and Exercise, American College of Sports Medicine; October 1986; Vol. 18; No. 5; pp. 489-500.
- Woo, Savio L.-Y. (ed.); Injury and Repair of the Musculoskeletal Soft Tissues;American Academy of Orthopaedic Surgeons; (1988); pp. 18-21; 106-117; 151-157.
- 28) Woo SL-Y, Richard E. Debski, Jennifer Zeminski, Steven D Abramowitch, Serena S Chan Saw, and James A Fenwick; Injury and Repair of Ligaments and Tendons; Annual Review of Biomedical Engineering; 2000; Vol. 2; pp. 83–118.
- Majno G, Jori I; Cells, Tissues, and Disease: Principles of General Pathology; Oxford University Press; 2004.
- Hildebrand KA, Gallant-Behm CL, Kydd AS, Hart DA; The Basics of Soft Tissue Healing and General Factors that Influence Such Healing; Sports Medicine Arthroscopic Review; September 2005; Vol. 13; No. 3; pp. 136–144.
- Walsh W; Orthopedic Biology and Medicine; Repair and Regeneration of Ligaments, Tendons, and Joint Capsule; Orthopedic Research Laboratory, University of New South Wales, Sydney, Australia; Humana Press; 2006.
- Schleip R; Fascia; The Tensional Network of the Human Body; The Scientific and Clinical Applications in Manual and Movement Therapy; Churchill Livingstone; 2012.
- Hauser RA, Dolan EE, Phillips HJ, Newlin AC, Moore RE, Woldin BA; Ligament Injury and Healing: A Review of Current Clinical Diagnostics and Therapeutics; The Open Rehabilitation Journal; 2013; No. 6; pp. 1-20.
- Stearns ML; Studies on development of connective tissue in transparent chambers in rabbit’s ear; American Journal of Anatomy; Vol. 67; 1940; p. 55.
- Kannus P; Immobilization or Early Mobilization After an Acute Soft-Tissue Injury?; The Physician And Sports Medicine; March, 2000; Vol. 26; No. 3; pp. 55-63.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”