Cervical Versus Lumbar
Intervertebral Discs
The Anatomical, Clinical,
and Management Distinctions
The Cervical Disc is
NOT a Mini Lumbar Disc
Most of what is understood and taught about the intervertebral discs was ascertained by studying the lumbar discs. The “era of the intervertebral disc” began in 1934 when William Jason Mixter and Joseph Seaton Barr read their paper, Rupture of the Intervertebral Disc with Involvement of the Spinal Canal, to the Annual Meeting of the New England Surgical Society (1). Dr. Mixter was then Chief of Neurosurgery at Massachusetts General Hospital and Professor of Neurosurgery at Harvard Medical School. Dr. Barr was then Orthopedic Surgeon to Outpatients at Massachusetts General Hospital.
Since 1934, the terminology pertaining to lumbar spinal disc herniations has been confusing, inconsistent, and contradictory. In 2014, the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology convened a combined task force to agree upon the nomenclature (2). Their consensus includes:
The Normal Disc 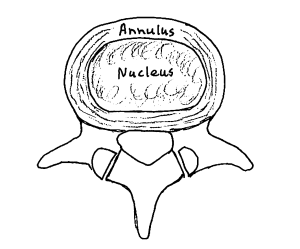
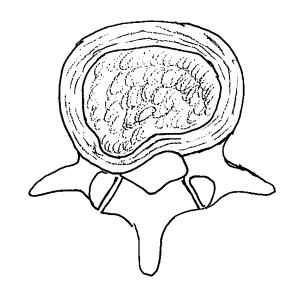
The Bulging Disc
If any part of the annulus extends beyond the normal disc space, it is considered to be a bulging disc.
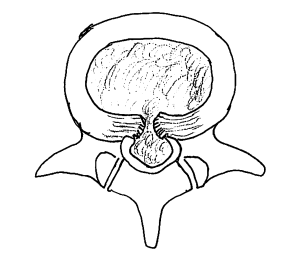
The Protrusion Disc
In the protrusion disc, the base of the displaced material is greater than the distance the disc material had moved towards the intervertebral foramen and/or the central neural canal.
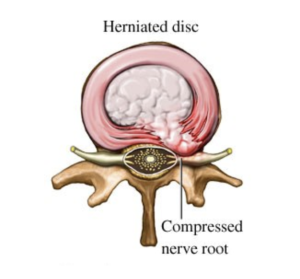
The Extrusion Disc
In the extrusion disc, the greatest measure of the displaced disc material is greater than the measure of the base of the displaced material.
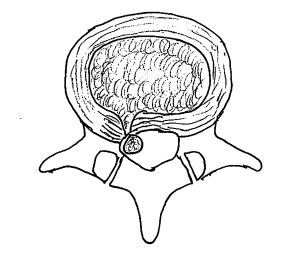
The Sequestration Disc
In the sequestration disc, the disc material has lost all connection with the original disc material.
This nomenclature of the intervertebral disc is dependent upon a distinct anatomical difference between the nucleus pulposus and the annulus fibrosis.
The nucleus pulposus (“nucleus”) is at the center of the disc. The nucleus is mostly water and functions as a ball-bearing, allowing the vertebrae to bend and twist. The annulus fibrosis (“annulus”) surrounds the nucleus. The annulus fibers are tough, dense, and strong. The annulus fibers surround the nucleus (3, 4).
With age, the water content of the nucleus diminishes, and the nucleus gradually becomes much more like the annulus in consistency. As such, herniation of the intervertebral discs is much more common in youth and less common as people age.
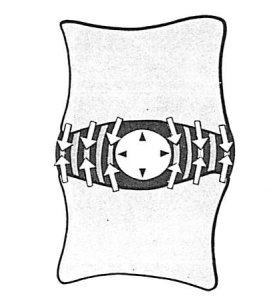
Also, with age, acute injury, or repetitive stress, the fibers of the annulus can degrade, allowing for the types of herniations shown above. When the nucleus moves in a posterior (backwards) direction, it may put pressure on the nerve root, the cauda equina, or the spinal cord (3, 4).
Although decompressive surgery is occasionally necessary, there is no doubt that spinal manipulation and chiropractic care is an effective conservative treatment for low back disc herniation with compressive neuropathology (5, 6, 7, 8, 9, 10, 11, 12, 13, 14).
•••••••••
Academics and clinicians often assume that the anatomy of the cervical intervertebral disc is similar, if not identical, to that of the lumbar spine. The cervical disc is often viewed as a small lumbar disc. Yet, dissension to this began to appear in the orthopedic literature more than 30 years ago.
In 1988, the journal Spine published a study titled (15):
Intervertebral Disc Changes
with Aging of Human Cervical Vertebra:
From the Neonate to the Eighties
The authors are from the department of Orthopaedic Surgery, Saitama Medical Center, Japan. They note that the “intervertebral disc is one of the most important structures in the maintenance of spinal function.” Yet, “histologic observations of the aging process of the cervical discs have been reported only in small numbers.”
Their study of the cervical discs used 155 human cadavers with ages ranging from six days to the ninth decade. The primary cause of death was cardiovascular disease. None of the subjects’ deaths were related to cervical spinal disease. All specimens were stained and evaluated histologically with an optical microscope. Special emphasis was given to the age changes in the nucleus pulposus.
The age groupings for the specimens were:
- Less than 1 year of age: 4
- Ages 2-12: 8
- Ages 13-19: 4
- Ages 20-30: 38
- Ages 40-50: 40
- Ages 60-90: 61
The authors’ findings included:
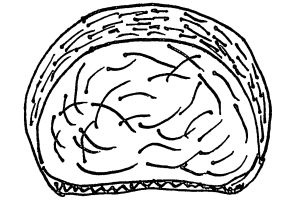
- In infants under 1-year of age, the nucleus was a gelatinous matrix surrounded by dense fibrous tissue.
- In specimens aged 1 to 12 years, the main cells of the nucleus pulposus “became sparse with aging, and fine fibrous tissue occupied most of the nucleus pulposus.”
- In the teenage years, most of the nucleus pulposus had been replaced by fibrous tissue.
- In specimens older than 20 years, “the nucleus pulposus had been replaced by fibrocartilage and dense fibrous tissue.”
The authors concluded:
“The infantile type of nucleus pulposus, containing cells originating from the notochord and surrounded by a fine fibrous tissue, was replaced by the adult type with a firmer structure, composed of fibrocartilage and dense fibrous tissue at the first half of the second decade.”
“The adult nucleus pulposus is composed of fibrocartilage and fiber components, in distinct contrast with the gelatinous nature of the disc of childhood.”
••••
In 1990, the journal Seminars in Arthritis Rheumatism published a study titled (16):
Anatomy and Physiology of the Cervical Spine
The primary author, John Bland, MD, was Professor of Medicine and Rheumatology at the University of Vermont College of Medicine (d. 2008, age 90 years).
Dr. Bland and colleague noted that the lumbar spine had been extensively studied since 1934, but that “the cervical spine had received far less attention.” They state:
“Anatomic, physiological, biochemical, and biomechanical characteristics of the lumbar spine are often presumed to apply to the cervical spine. The differences are far too extensive to warrant such an assumed correlation.”
This paper is based on 171 whole human spines they had studied anatomically, physiologically, and histologically. Their findings include:
“The nuclei pulposi of the cervical intervertebral discs, present at birth, are progressively less evident in adolescence, and by age 40 years have disappeared.”
“The adult disc is ligamentous-like, ‘dry,’ and composed of fibrocartilage, islands of hyaline cartilage, and tendon-like material, with little or no proteoglycans.”
“Thus, after age 40 years, it is impossible to clinically herniate the nucleus pulposus as there is none.”
••••
Dr. Bland wrote a book pertaining to the cervical spine titled (17):
Disorders of the Cervical Spine, Diagnosis and Management
In the second edition, published in 1994, Dr. Bland had expanded his 171 cervical spine specimen study to 191 specimens. He notes:
“The nucleus pulposus, present at birth, and remaining until age 9 to 14 years, is made of remnants of primitive notochord and proteoglycan material.”
“However, in the cervical spine, contrary to events in the lumbar spine, the nucleus pulposus gradually disappears.”
“In 191 whole human cervical spines, we found no evidence of a gel-like nucleus pulposus after age 45.”
“The intervertebral disc in the cervical spine is ‘dry,’ more like ligament than ‘disc,’ fibrous, and gradually breaking up in various sized pieces, seemingly a universal, probably physiological, development.”
••••
In 1999, the journal Spine published a study titled (18):
The Ligaments and Annulus Fibrosus of Human Adult
Cervical Intervertebral Discs
The primary author, Susan Mercer, PhD, is from the Department of Anatomy and Structural Biology, University of Otago, Dunedin, New Zealand. The objective of this microdissection study was to determine the morphology of the human adult cervical intervertebral disc and its ligaments. The authors note that “a detailed three-dimensional description of the cervical intervertebral disc and its surrounding ligaments is currently unavailable.” This is concerning because “some studies indicate that the cervical disc is distinctly different from the lumbar intervertebral disc, yet most clinical and anatomic texts appear content with extrapolating data from the lumbar spine.”
The authors state:
“Fundamental to any appreciation of the mechanism causing injury to the cervical intervertebral disc is a knowledge of their normal structure.”
The authors used whole cervical spines from 12 human adult cadavers.
Using microdissection, the ligaments and the fibrous components of 59 cervical intervertebral discs were resected systematically.
FINDINGS
Axial View Cervical Disc
Viewed From Above
Anterior
Posterior
- “The cervical anulus fibrosus does not consist of concentric laminae of collagen fibers as in lumbar discs.”
- “Instead, it forms a crescentic mass of collagen thick anteriorly and tapering laterally toward the uncinate processes.” It is essentially deficient posteriorly and laterally.
- “The three-dimensional architecture of the cervical anulus fibrosus is more like a crescentic anterior interosseous ligament than a ring of fibers.”
KEY COMMENT
The authors discovered that the “nucleus” consisted of a “deep core of undissectable fibrocartilaginous material.” They state:
“The development of cervical discs is distinctly different from that of the lumbar discs. The nucleus at birth constitutes no more than 25% of the entire disc, not the 50% as in the lumbar discs.”
“With aging, the nucleus pulposus rapidly undergoes fibrosis such that by the third decade [20-30 years] there is barely any nuclear material distinguishable.”
SUMMARY COMMENTS
“Readers may be startled as the investigators were by the results of this study: the structure of the cervical discs does not match the descriptions they have currently received in literature.”
“The cervical discs are not like lumbar discs.”
“Skeptical individuals might argue that the current study was confounded by the use of elderly cadavers and that features observed were the consequence of degenerative or age-related changes. However, all of the specimens exhibited the same morphology including the sample taken from the 39-year-old individual and the two other individuals younger than 50 years of age.”
“The different anatomy of the cervical annulus fibrosis means that the model devised for lumbar discs cannot be applied to the neck. A separate and new model must be devised for the cervical discs.”
••••
Nikolai Bogduk is a unique individual. As of January 2022, PUBMED, the search engine for the US National Library of Medicine, locates 302 articles using his name. Dr. Bogduk is currently Emeritus Professor of Pain Medicine at the University of Newcastle, NSW, Australia. Dr. Bogduk holds an MD, PhD, and ScD. In addition:
- He began research into spinal pain in 1972, when essentially nothing was known about the problem.
- His anatomical studies have become the basis of clinical applications.
- He developed and tested new diagnostic and surgical procedures for back pain and for neck pain.
- He is a consultant for the International Spine Intervention Society for various studies of spinal diagnostic and treatment procedures.
- He developed and tested evidence-based practice guidelines for the management of back pain, neck pain, shoulder pain, knee pain, and pain in the foot, wrist, and elbow.
- He has been awarded the Volvo Award for Back Pain Research, the Research Prize of the Cervical Spine Research Society, the Award for Outstanding Research of the North American Spine Society, and three times the Research Prize of the Spine Society of Australia.
- He is on the editorial board of the journal Pain Medicine.
- He conducted studies on the normal and abnormal biomechanics of the spine, which have now become pertinent to the evaluation of arthroplastic surgery of the spine.
- He performed anatomical studies and clinical trials to disprove myths in medical practice.
- He has taught at all academic levels, from tutor to professor, in classical and problem-based learning systems.
- He has taught undergraduates in all health disciplines.
- He has taught postgraduate surgeons.
- He has regularly been a keynote speaker at health profession conferences internationally.
- He has served on the Academic Boards or Senates of three universities.
- He has been an Assistant Dean in the Faculty of Medicine.
- He is on the Editorial Board of Cephalalgia, Journal of the International Headache Society.
- He is the Editor of Pain Medicine, Official Journal of American Academy of Pain Medicine.
- He is fluent in English, French, and Russian.
Dr. Bogduk is the most noted, respected, and influential clinical anatomist of our time, and perhaps of all history.
In 2012, the journal Radiological Clinics of North America published a study, authored by Dr. Bogduk, titled (19):
Degenerative Joint Disease of the Spine
In this article, Dr. Bogduk integrates spinal articular metabolic disturbances, genetic factors, age, and physical loading contributions to spinal degenerative joint disease and to spinal pain syndrome. Importantly, he makes these observations:
“Cervical disks differ from lumbar disks in their anatomic structure and their expression of degenerative changes.”
“At a microscopic level, the structure and biomechanics of joints in the cervical spine and lumbar spines differ.”
“Cervical disks lack a concentric anulus fibrosus; the anulus is well developed only anteriorly, where it serves more as an interosseous ligament, and not as a circumferential constraint around the nucleus.”
“The nucleus pulposus is relatively small at birth and persists until the second decade of life [10-20 years], but thereafter it gradually disappears, leaving a firm, dry plate of fibrocartilaginous bulges and osteophytes.”
CONCLUSIONS
The studies presented here question the ability of the cervical disc to herniate and create compressive neuropathology, especially after the ages 20-40 years. In addition to these findings, there is good evidence that chiropractic spinal adjusting (specific line-of-drive manipulation) is both safe and effective for the management of cervical spine radiculopathy (20).
REFERENCES
- Mixter WJ, Barr JS; Rupture of the Intervertebral Disc with Involvement of the Spinal Canal; New England Journal of Medicine; August 2, 1934; Vol. 211; pp. 210–215.
- Fardon DR, Williams LA, Dohring EJ, Rothan SL, Sze GK; Lumbar Disc Nomenclature: Version 2.0: Recommendations of the Combined task forces of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology; Spine Journal; November 1, 2014; Vol. 14; No. 11; pp. 2525-2545.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second edition; JB Lippincott Company; 1990.
- Kapandji AI; The Physiology of the Joints: The Spinal Column, Pelvic Girdle and Head; Seventh Edition; Handspring Publishing; 2019.
- Ramsey RH; Conservative Treatment of Intervertebral Disk Lesions; American Academy of Orthopedic Surgeons, Instructional Course Lectures; Vol. 11; 1954; pp.118-120.
- Mathews JA, Yates DAH; Reduction of Lumbar Disc Prolapse by Manipulation; British Medical Journal; September 20, 1969; No. 3; 696-697.
- Edwards BC; Low back pain and pain resulting from lumbar spine conditions: A comparison of treatment results; Australian Journal of Physiotherapy; September 1969; Vol. 15; No. 3; pp. 104-110.
- Turek S; Orthopaedics, Principles and Their Applications; JB Lippincott Company; 1977; page 1335.
- Kuo PP, Loh ZC; Treatment of Lumbar Intervertebral Disc Protrusions by Manipulation; Clinical Orthopedics and Related Research; February 1987; No. 215; pp. 47-55.
- White AA, Panjabi MM; Clinical Biomechanics of the Spine; Second edition; JB Lippincott Company; 1990.
- Cassidy JD, Thiel HW, Kirkaldy-Willis WH; Side posture manipulation for lumbar intervertebral disk herniation; Journal of Manipulative and Physiological Therapeutics; February 1993; Vol. 16; No. 2; pp. 96-103.
- Santilli V, Beghi E, Finucci S; Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: A randomized double-blind clinical trial of active and simulated spinal manipulations; The Spine Journal; March-April 2006; Vol. 6; No. 2; pp. 131–137.
- Leemann S, Peterson KP, Schmid C, Anklin B, Humphreys BK; Outcomes of Acute and Chronic Patients with Magnetic Resonance Imaging–Confirmed Symptomatic Lumbar Disc Herniations Receiving High-Velocity, Low-Amplitude, Spinal Manipulative Therapy: A Prospective Observational Cohort Study with One-Year Follow-Up; Journal of Manipulative and Physiological Therapeutics; March/April 2014; Vol. 37; No. 3; pp. 155-163.
- Deyo R, Mirza S; Herniated Lumbar Intervertebral Disk; New England Journal of Medicine; May 5, 2016; Vol. 374; No. 18; pp. 1763-1772.
- Oda j, Tanaka H, Tsuzuki N; Intervertebral disc changes with aging of human cervical vertebra. From the neonate to the eighties; Spine; November 1988; Vol. 13; No. 11; pp. 1205-1211.
- Bland JH, Boushey DR; Anatomy and Physiology of the Cervical Spine; Seminars in Arthritis and Rheumatism; August 1990; Vol. 20; No. 1; pp. 1-20.
- Bland JH; Disorders of the Cervical Spine, Diagnosis and Management; Second Edition; WB Saunders Company; 1994; p. 73.
- Mercer S, Bogduk N; The Ligaments and Annulus Fibrosus of Human Adult Cervical Intervertebral Discs; Spine; April 1, 1999; Vol. 24; No. 7; pp. 619-628.
- Bogduk N; Degenerative Joint Disease of the Spine; Radiological Clinics of North America; July 2012; Vol. 50; No. 4; pp. 613-628.
- Peterson CK, Schmid C, Leemann S, Anklin B, DC; Humphreys BK; Outcomes from Magnetic Resonance Imaging: Confirmed Symptomatic Cervical Disk Herniation Patients Treated with High-Velocity, Low-Amplitude Spinal Manipulation Therapy: A Prospective Cohort Study With 3-Month Follow-Up; Journal of Manipulative and Therapeutics; October 2013; Vol. 36; No. 8; pp. 461-467.
“Authored by Dan Murphy, D.C.. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”