The Cervical Spine and Tinnitus
A classification method for nerves is to distinguish them as either spinal nerves or cranial nerves:
- Spinal nerves exit/enter the spinal cord via the intervertebral foramen between two adjacent spinal vertebrae.
- Cranial nerves exit/enter the brainstem and/or brain via the skull (cranial nerve XI, the spinal accessory nerve, is an exception: it is fully formed from neck nerve roots that enter and exit the skull).
Of the twelve cranial nerves, one is anatomically/physiologically unique because is conveys two distinct functions. This nerve is the vestibulocochlear nerve, or cranial nerve (CN) VIII. They are the vestibular nerve (for balance) and the cochlear (auditory) nerve (for hearing). Although these nerves travel together, they convey different modalities.
The vestibular nerve conveys information related to motion and position (1). Typical symptoms relayed by the vestibular nerve include dizziness, vertigo, spinning, lightheadedness, and unsteadiness.
The cochlear nerve conveys normal sounds, typical hearing. The cochlear nerve also conveys abnormal sounds known as tinnitus. Typically, tinnitus is experiencing ringing or other noises in the ears (2). The noise of tinnitus is not caused by an external source, and other people cannot hear it.
The primary subject of this discussion is the cochlear portion of CN VIII and tinnitus. Specifically, this discussion presents information on how cervical spine nerves (neck nerves) can cause tinnitus (cranial nerve VIII) and how chiropractic care of the spine can benefit patients suffering from tinnitus.
•••••
Basic Neurophysiology
The perception of sound, including tinnitus, is an electrical signal interpreted by the brain. The sound (tinnitus) electrical signal is brought to the brain by nerves. The sound (tinnitus) nerve is the cochlear nerve portion of the vestibulocochlear nerve, also known as cranial nerve VIII (CN VIII).
Sound waves in the air (like a tree falling in the woods, the vibrations emanating from a musical instrument, or the vibrations being generated by a friend’s voice, etc.) are converted to the sound electrical signal that the brain can perceive in a spot in the inner ear called the cochlea.
The electrical signals that are generated in the cochlea do not go directly, nonstop, to the part of the brain that interprets them (the auditory cortex). Rather, there are five stops where the electrical signal can be modified (enhanced or suppressed). These stops are also known as synapses. The first synapse for the electrical signal generated by the cochlea is located in the brain stem.
A typical sequence for these stops (somewhat oversimplified) would be as follows: Sound Waves (Mechanical Vibrations from the Environment) → Cochlea (inner ear, Where Sound Waves are Converted to Electrical Signals) → Dorsal Cochlear Nucleus (The Primary Concern for this Presentation) → Superior Olivary Nucleus → Inferior Colliculus → Medial Geniculate Body → Brain’s Auditory Cortex (For Sound Perception and Interpretation)
This discussion primarily involves the Dorsal Cochlear Nucleus. The dorsal cochlear nucleus is the first synaptic relay in the brainstem after the sound electrical signals are generated in the cochlea of the inner ear (1, 2).
Anatomical Considerations
Neck structures (muscles, ligaments, discs, facet, etc.) are innervated by cervical (neck) spine nerve roots. For about 5 decades, publications have documented that cervical spine problems in alignment, inflammation, irritation, compression, instability, etc., have the ability to cause tinnitus. A literature search of the United States National Library of Medicine using PubMed identified 33 publications using the terms “cervicogenic tinnitus.”
One of the studies was published in the German journal HNO [Ears Nose Throat] in 1994 (3):
“HNO is an internationally recognized journal and addresses all ENT [ears nose throat] specialists in practices and clinics dealing with all aspects of ENT medicine, e.g. prevention, diagnostic methods, complication management, modern therapy strategies and surgical procedures.”
Although the article was titled “Cervicogenic Hearing Loss,” the author notes that the hearing loss is often accompanied with tinnitus. The journal is published in German (from the University of Heidelberg), but the English abstract includes:
“[Vertebrogenic hearing loss] is believed accompanied by tinnitus, a feeling of ear pressure, otalgia and deafness as symptoms of a functional deficit of the upper cervical spine.”
“Findings in 62 patients suffering from vertebragenic hearing disorders are reported before and after chiropractic management.”
“Results indicate that these hearing disorders are reversible.”
“The therapy of choice is chiropractic manipulation of the upper cervical spine.”
It is important to note the advocacy of the use of chiropractic manipulation on this patient population.
A common theme in these articles of cervicogenic tinnitus include:
- The involvement of the dorsal cochlear nucleus (4, 5, 6, 7, 8, 9, 10).
- That the dorsal cochlear nucleus receives inputs from various cervical spine tissues, transmitted by the cervical nerve roots.
- A variety of clinical interventions that target cervical spine structures have been shown to help people suffering from cervicogenic tinnitus, including chiropractic care.
Below, some representative studies are summarized.
•••••
In 1998, a study was published in the International Tinnitus Journal, titled (11):
The Influence of Atlas Therapy on Tinnitus
The author proposes that the proprioceptive input from the small posterior cervical muscles to the brainstem are a source of tinnitus. For management, he advocates for “atlas therapy.” The goal of atlas therapy is to cause a reflex inhibition of hypertonic posterior cervical spine musculature. Simultaneously, “atlas therapy” will influence the neurological input to the brainstem. Theoretically, this could influence the brainstem dorsal cochlear nucleus.
“Atlas therapy” is done by “applying specific force to the wing of the atlas, the first vertebra.” The author also notes that this maneuver is often “attempted by chiropractors.”
The author presents a series of 11 post-traumatic tinnitus patients who were treated with “atlas therapy.” The outcomes were:
- 7 patients experienced a complete recovery
- 3 patients showed improvement
- 1 patient did not benefit
The author states:
“If the input to the brainstem is normalized by atlas therapy, the problem can be resolved.”
•••••
In 2013, a study was published in the Journal of the American Academy of Audiology, titled (12)
Improving Tinnitus with Mechanical Treatment of the Cervical Spine and Jaw
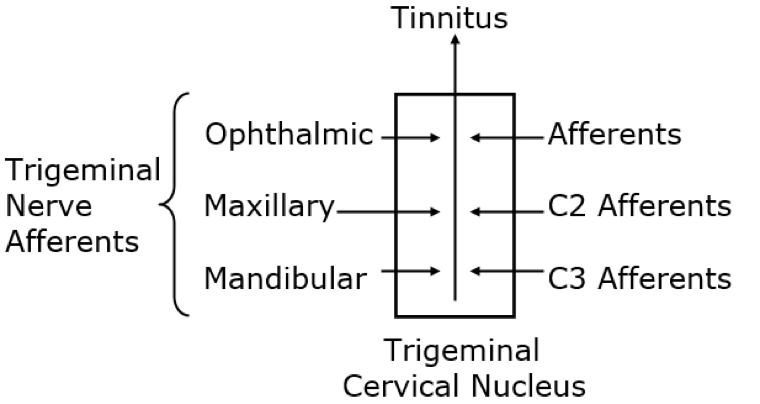
It should be understood that the cervical spine and the jaw share neurological input into the brainstem (13, 14). The point of convergence is termed the trigeminal cervical nucleus. Upper cervical spine nerves and the tissues they innervate send afferent information into the trigeminal cervical nucleus; this nucleus also receives input from the trigeminal nerve (CN V).
The trigeminal nerve is comprised of three branches:
- Ophthalmic
- Maxillary
- Mandibular
The mandibular branch innervates the temporomandibular joint.
The authors of this study (12) are from the Neurological Institute, Cleveland Clinic, Cleveland, OH. They describe a case of a 42-year-old male auto mechanic experiencing intermittent bilateral tinnitus and several other symptoms. The patient described his tinnitus as a “buzzing.” The patient attributed his symptoms to prolonged positions of head protrusion and neck flexion while working as a mechanic.
In agreement with most studies, the authors agree that tinnitus is associated with hyperactivity in the dorsal cochlear nucleus, and that somatosensory and auditory interactions occur in the dorsal cochlear nucleus. Here, auditory neurons receive direct input not only from the cochlear nerve, but also from inputs from the cervical nerves that innervate the muscles of the neck and from the trigeminal nucleus, whose inputs come from nerves innervating the muscles of the face and jaw. The authors state:
“Musculature and joint pathologies of the head and neck are frequently associated with tinnitus.”
“There are strong indications that a connection exists between tinnitus, neck pain, and jaw disorders.”
“Abnormalities of the cervical spine, specifically the upper cervical spine mobility and the cervical spine musculature, might be somatic factors contributing to this patient’s tinnitus. There was also suspicion that the jaw might be a secondary contributor.”
“Tinnitus is commonly associated with temporomandibular disorders and upper cervical dysfunction.”
“Cranio-cervical posture defects have been coupled with TMD and myofascial pain to the neck and jaw muscles, and treatment targeted to the TMJ has been shown to reduce complaints of cervicogenic headache.”
The authors note that mechanical care of the temporomandibular joint, acupuncture, and “resolving vertebral subluxations” [chiropractic care] have “been reported to be of benefit to patients with tinnitus.” They state:
“The ability to modulate tinnitus in human subjects by manipulations of head and neck muscles has been well described and is referred to as somatic tinnitus.”
Examination of this patient found reductions in cervical ranges of motion in extension, bilateral rotation, and lateral flexion. Also, asymmetry was noted in his temporomandibular joint (TMJ) movements.
His treatment focused on normalizing cervical spine mobility through repetitive movements, joint mobilization, and soft tissue massage. Ten in-clinic patient visits were given. At the end of these treatment sessions, the patient demonstrated a complete reversal of his tinnitus.
Home treatment included repeated posture-improving movements and augmented self-mobilization techniques to “correct the limitation of his upper cervical rotation (C1-C2).”
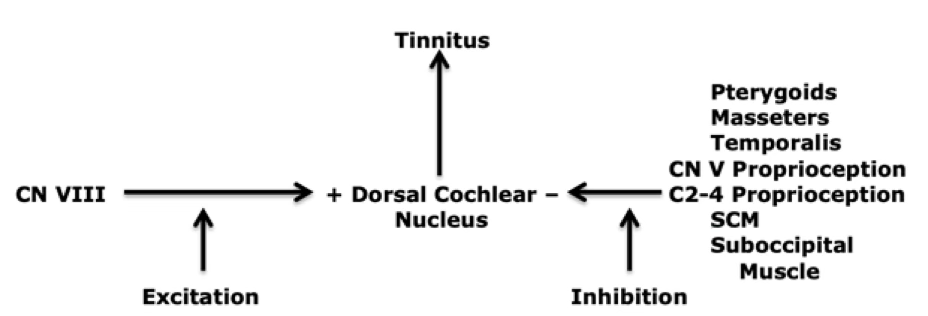
The authors propose that improvements in muscle and joint function of the upper cervical spine and the temporomandibular joint improves the proprioceptive input that inhibits the dorsal cochlear nucleus tinnitus signal.
The authors suggest that the most important spinal nerve root as related to tinnitus is C2. Disruption or loss of normal input from C2 may result in loss of inhibitory interneurons, resulting in disinhibition and the emergence of tinnitus-producing hyperactivity. The authors state:
“Therapy designed to restore balance of muscle tonicity in the neck could restore normal activity in C2, thereby reversing the dis-inhibitory process; this reversal of disinhibition may then abolish tinnitus by restoring normal levels of activity in fusiform cells.”
The authors summarize that a tinnitus treatment approach targeting the upper cervical spine, cervical muscles, and the temporomandibular joint (TMJ) can reduce or abolish tinnitus perception. They state:
“This case reflected treatment targeted at cervical and TMJ impairments and notable improvements to tinnitus.”
This study shows the neurological inhibitory benefits of improved upper cervical biomechanical function.
•••••
In 2024, an article was published in the journal Cureus, titled (15):
Cervicogenic Somatic Tinnitus:
A Narrative Review Exploring Non-otologic Causes
The authors reaffirm that cervicogenic somatic tinnitus (CST) arises from altered sensory input from the cervical spine. The typical sources for the altered sensory input include degenerative disc disease, cervical spondylosis, whiplash injuries, and neck muscle stress or spasms.
The authors also note that the dorsal cochlear nucleus (DCN) in the brainstem plays a crucial role in cervicogenic somatic tinnitus because it receives input from both the cochlear nerve and from cervical spine structures. This agrees with the above studies presented here.
The authors note that there are associations between tinnitus and cervical spine pathologies, neck myofascial tightness, or cervical neck instability. They state:
“The pathophysiology of CST involves complex interactions between the cervical spine’s somatosensory inputs and central auditory pathways, particularly affecting the dorsal cochlear nucleus (DCN) in the brainstem, leading to enhanced excitability and synaptic reorganization, giving rise to tinnitus.”
“The dorsal cochlear nucleus (DCN) in the brainstem, which receives input from the auditory nerve, plays a crucial role in the development of tinnitus.”
“Prolonged aberrant somatosensory input from the cervical spine can lead to enhanced excitability and reorganization of synapses in the DCN, sustaining tinnitus perception even without ongoing cervical spine impairment.”
“The involvement of the dorsal root ganglia of the second, seventh, and eighth cervical nerves, along with the trigeminal ganglion, establishes connections with the auditory system.”
“Proprioceptive and nociceptive inputs from the cervical spine influence neuronal regions in the brainstem related to hearing.”
“Assessing the patient’s posture and feeling for trigger points or spasms in the neck muscles are important tasks for the clinician.”
The authors suggest that in the evaluation of cervicogenic somatic tinnitus, standard cervical spine testing should be included. They recommend:
- Cervical spine X-rays, which can detect structural anomalies, spondylosis, degenerative disc disease, and misalignments.
- Computed Tomography (CT) to identify facet joint arthrosis and cervical spine osteophytes.
- MRI imaging to assess the intervertebral discs, spinal cord, and nerve roots.
- “The diagnosis of CST is mostly dependent on imaging studies.”
For the management of cervicogenic somatic tinnitus, the authors emphasize the importance of relieving musculoskeletal tension and restoring the cervical spine to its natural function. They specifically state:
“By reducing muscular tension and cervical spine stiffness, techniques such as joint mobilization, manipulation, and soft tissue massage might lessen aberrant somatosensory input to the auditory pathways.”
The authors advocate for the use of chiropractic to address cervical spine dysfunctions and related soft tissue disorders. They state:
“Chiropractic adjustments work by treating spinal misalignments and enhancing cervical spine function.”
“Chiropractors frequently use high-velocity thrusts to manipulate the spine, targeting a particular cervical joint. By using this method, joint misalignments can be corrected, nerve irritation can be decreased, and normal joint mechanics can be restored.”
In further support of the chiropractic approach in the management of cervicogenic somatic tinnitus, the authors state:
“Joint mobilization and manipulation can enhance joint function, lessen pain, and improve mobility.”
“A key component of treating CST is manual therapy, which aims to relieve musculoskeletal stress and return the cervical spine to normal function.”
“Understanding the underlying somatosensory mechanisms of the proprioceptive and nociceptive innervated structures in the head and neck regions (joints, muscles, ligaments, fasciae, and spinal and peripheral nerves), as well as dysregulated nociceptive processing in the central nervous system regarding the hypersensitivity of the DCN, is the first step toward offering manual therapy as a treatment option.”
“Reducing aberrant somatosensory input from the cervical region to the auditory pathways is manual therapy’s main objective, which helps mitigate tinnitus symptoms.”
“Cervical traction may decompress the cervical vertebrae and lessen pressure on the spinal nerves. This method can enhance cervical spine alignment and reduce pain.”
“Better circulation, brought on by manual therapy, supports the general health of the cervical spine by removing metabolic waste products and nourishing tissues. It can have a neuro-modulatory effect by adjusting sensory inputs at the cervical level, which may lessen the severity and frequency of tinnitus.”
“Manual therapy is essential for treating cervical spine dysfunctions that lead to aberrant somatosensory input in cases of CST.”
“Manual therapy can alleviate discomfort, increase cervical mobility, lessen muscle tension, and improve the general health of the cervical spine using methods such as joint mobilization, soft tissue mobilization, and cervical traction.”
“Manual therapy has the potential to greatly enhance the quality of life and lessen tinnitus symptoms for individuals with CST when included in an all-encompassing treatment approach.”
Summary Comments
When a patient presents with tinnitus, health care providers, including chiropractors, have an immediate concern for the potential of a vascular etiology. For chiropractors, the most concerning vascular relationship is the blood delivered to the dorsal cochlear nucleus via the vertebral artery. History and examination of the patient should increase or decrease vascular etiology suspicions.
This presentation makes it clear that many cervical spine tissues and nerves can cause tinnitus, and that appropriate mechanical care, including chiropractic adjustments, are often beneficial for many patients.
The bottom line is that all patients presenting with tinnitus should have a thorough evaluation of cervical spine structures and appropriate mechanical-based care should be used in its management.
REFERENCES
- Bordoni B, Mankowski NL, Daly DT; Neuroanatomy: Cranial Nerve 8 (Vestibulocochlear); StatPearls; May 22, 2023.
- Wilson-Pauwels L, Stewart PA, Akesson EJ, Spacey SD; Cranial Nerves, Function & Dysfunction; Third edition; People’s Medical Publishing House; 2010.
- Hulse M; Cervicogenic Hearing Loss; HNO; October 1994; Vol. 42; No. 10; pp. 604-613.
- Levine RA; Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis; American Journal of Otolaryngology; November-December 1999; Vol. 20; pp. 351-362.
- Kaltenbach JA, Zhang J, Finlayson P: Tinnitus as a plastic phenomenon and its possible neural underpinnings in the dorsal cochlear nucleus; Hearing Research; August 2005; Vol. 206; No. 1; pp. 200-226.
- Zhan X, Pongstaporn T, Ryugo DK; Projections of the second cervical dorsal root ganglion to the cochlear nucleus in rats; Journal of Comparative Neurology; May 2006; Vol 496; No. 3; pp. 335-348.
- Shore SE, Koehler S, Oldakowski M, Hughes LF, Syed S; Dorsal cochlear nucleus responses to somatosensory stimulation are enhanced after noise-induced hearing loss; European Journal of Neuroscience; January 2008; Vol. 27; No. 1; pp. 155-168.
- Dehmel S, Cui YL, Shore SE; Cross-modal interactions of auditory and somatic inputs in the brainstem and midbrain and their imbalance in tinnitus and deafness; American Journal of Audiology; December 2008; Vol. 17; No. 2; pp. 193-209.
- Shore SE; Plasticity of somatosensory inputs to the cochlear nucleus: Implications for tinnitus; Hearing Research; November 2011; Vol. 281; No. 1-2; pp. 38-46.
- Wu C, Martel DT, Shore SE: Increased synchrony and bursting of dorsal cochlear nucleus fusiform cells correlate with tinnitus; Journal of Neuroscience; February 10, 2016; Vol. 36; No. 6; pp. 2068-2073.
- Kaute BB; The Influence of Atlas Therapy on Tinnitus; International Tinnitus Journal; 1998; Vol. 4; No. 2; pp. 165-167.
- Cherian K, Cherian N, Cook C, Kaltenbach JA; Improving Tinnitus with Mechanical Treatment of the Cervical Spine and Jaw; Journal of the American Academy of Audiology; July-August 2013; Vol. 24; No. 7; pp. 544-555.
- Kaplan AS, Assael LA; Temporomandibular Disorders: Diagnosis and Treatment; WB Saunders Company; 1991.
- Bogduk N; Anatomy and Physiology of Headache; Biomedicine and Pharmacotherapy; January 1999; Vol. 49; No. 10; pp. 435-445.
- Wadhwa S, Jain S, Patil N, Jungade S; Cervicogenic Somatic Tinnitus: A Narrative Review Exploring Non-otologic Causes; Cureus; July 26, 2024; Vol. 16; No. 7; pp. e65476.
“Authored by Dan Murphy, D.C. Published by ChiroTrust® – This publication is not meant to offer treatment advice or protocols. Cited material is not necessarily the opinion of the author or publisher.”